Medical editor
Global health producers
 BBC
BBCIt is 10 o’clock in the morning, and in more than two hours, Wayne Hawkins will die.
Suraj is shining at the bungalow, where 80 -year -old San Diego is a wife of more than five decades with his wife in California.
I knock at the door and meet their children – Emily, 48, and Ashley, 44 – who have spent the last two weeks in favor of their father.
Wayne sits on a recurrent chair where he spends most of his days. Terminal sick, he is very weak to leave home.
He has invited BBC News to witness his death under the Assisted Dyeing Lodge in California – because if the MPs in London voted to legalize the practice in England and Wales, it would allow some sick people to die in the same way here.
Half an hour after Wayne’s home, I see her swallowing three anti-Newsia bullets, designed to reduce the risk of vomiting the fatal drug that plan to take her soon.
Are you sure this day is your last, I ask him? “I am all inside,” he answers. “I was determined and decided weeks ago – I had not been fed up since then.”
His family asks for a last photo, which I take. As usual, Stella and Wayne are holding hands.
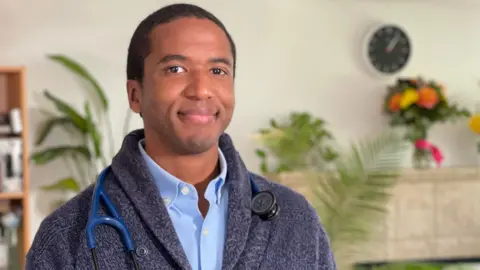
Shortly after, Dr. Doni Moore comes. He has come to know the family in the last few weeks, running the clinic of his own life and is visiting him on several occasions. Under the California Act, he is the one who is known as the attending physician, which should be confirmed, in addition to a second doctor, it is eligible for help in dying.
Dr. Moore’s role in this situation is Part Physician, Part Counselor, one is for the first 150 assisted deaths.
A brown glass bottle is seated on a top shelf in the bedroom of Wayne, which contains a good white powder – a mixture of five drugs, seditives and painkillers, transported to the house on the previous day. Dr. Moore explains that the dose of drugs is hundreds of times higher than people used in regular healthcare and “guarantee” to be fatal. Unlike California, the proposed law in Westminster will need a doctor to bring any such medicine with him.
When Wayne indicated that he is ready, the doctors mix the meds with cherry and pineapple juice to soften the bitter taste – and he hands over this pink liquid to the vein.
No one, the doctor, knows how long it will take to die after taking fatal medicines. Dr. Moore explains to me that, in his experience, death usually occurs between 30 minutes and two hours ingestion, but one occasion takes 17 hours.
This is the story of how and why Wayne chose to die. And why others have decided not to follow the same course.
We first met the couple a few weeks ago, when Wayne explained why he was going ahead with a controversial measure in other parts of the world – a supported death decision.
“A few days of pain is almost more than I can handle,” he said. “I just see any merit to die slow and painfully, bent with luggage – intubeshen, feeding tube,” he told me. “I do not want any of it.”
Wayne said that he had seen two relatives “unhappy”, “heinous” death with heart failure.
“I hate hospitals, they are sad. I will die on the road first.”
Wayne met Stella in 1969; The couple married four years later. He told us that it was something of a systematic marriage, as his mother continued to invite Steella to dinner until Penny was eventually dropped that he should take her out.
He lived in Arcata, Northern California for many years, surrounded by redwood trees, where Wayne served as a landscape architect, while Stella was a primary school teacher. He tried and camped his holidays with his children.
Now Wayne is ill with heart failure, which has already brought him closer to death. They have other health issues including prostate cancer, liver failure and sepsis that bring them severe spinal pain.
They have less than six months to live, qualifying them for a aided death in California. Their request to die is approved by two doctors and the fatal drug is self-influenced.
It was during our first meeting that he asked the BBC to return his last day to return, stating that he wanted the right to a aided death to a terminal sick adults in Britain.

“Britain is great with independence and it’s just one more,” he said. “People should be able to choose the time of their death as long as they fulfill the rules for living or less than.”
Stela, 78, supports her decision. “I have known him for more than 50 years. He is a very independent man. He always knows what he wants to do and he always cures things. How it is working now. If it is his choice, I definitely agree, and I have really seen him suffering from the disease that he has received. I don’t want to him.”
Wayne will also qualify under the newly aided dying law proposed in England and Wales. Measures return to the House of Commons later this month, when all MPs will have a chance to debate and vote in terminal sick adults (end of life) bills.
The proposed law presented by Labor MP Kim Leadbatter says that anyone who wants to end his life should have the mental ability to make an alternative, that they should expect to die within six months, and look at two different announcements – witnesses and signed – about the desire to die. They should satisfy two independent doctors that they are eligible.
MPs in Westminster voted in favor of assisted dyeing in theory last November, but were bitterly divided on the issue. If they eventually decide to approve the bill, it can be a law within the next year and can come into practice within the next four years.
There are also divisions in California, where assisted dyeing was introduced in 2016. Both Michelle and Mike Carter are married for 72 and 43 years, each is being treated for cancer – Mike has prostate cancer that has spread to their lymph nodes, and Mitchell’s advanced terminal ovarian cancer has spread to her body.
Mitchell told me, “When she passed, I held my mother’s hand; I held my father’s hand when he passed,” Mitchell told me. “I believe that there is freedom of choice for me, I choose to do solid care … I have God and I have a good medicine.”

Michelle’s doctor, Adhikak Karna Specialist Dr. Vincent Guyen argued that with the help of laws dying in the US state, there is “silent coercion”, which makes the weaker people feel that their only option is to die. “Instead of ending people’s lives, let’s put the program together to take care of the people,” he said. “Tell them that they are loved, they want and they are worthy.”
He said that the law means that doctors have gone from being seen as killers in the form of heellers, while the message from the healthcare system was that “you are better dead, because you are expensive and your death is cheap for us”.
Some disability campaigners say assisted dyeing makes them feel insecure. The Ingrid Tisher, who has muscle dystrophy and chronic respiratory failure, told me: “This message that sends people in California to people in California, is that you deserve suicidal aid instead of prevention of suicide when you wish to end your life.
“What does it say that we are as a culture?”
Critics often say that once it is helped to die once, the security measures around such laws over time are wiped out more comfortably as part of the “slippery slope” towards the criteria. In California, initially there was a 15-day cooling period between patients with the first and second request to help dying. This has decreased by 48 hours as many patients were dying during the waiting period. It is thought that the approval process envisaged in Westminster will take a month.
‘Goodbye,’ Wayne tells his family
Outside the house of Wayne on the morning of his death, a solitary bird begins its loud and wide song. “There is a mockingbird out that there is a mockingbird,” Ven tells Stella, as flickering on her face smiling.
Wayne hates the bird because it keeps it awake at night, stella jokes, one side of his chair in hand. Emily and Ashley are next to Stella.
Dr. sitting on the other side of Wayne. Moore handed him a pink liquid, which he swallows without any hesitation. “Good night,” he says to his family – a specific touch of humor from a person who told us that he was firm to die on his own terms. This is 11.47am.
After two minutes, Wayne says she is feeling sleepy. Dr. Moore asked her to imagine that she is running in a huge sea of flowers with a soft air on her skin, which seems suitable for a patient who spent most of her life among nature.
After three minutes, Wayne enters a deep sleep so that he will never wake up. On some occasions he raises his head to take a deep breath without opening his eyes, begins to snore gently at one point.
Dr. The Moore tells the family that it is “deepest sleep imaginative” and assures Emily that her father has no chance to wake up and ask, “Does it work?”
“Oh, it would be like him,” Stela says with a laugh.

The family starts reminding about the hiking of the holidays and driving around in a large van that they change to become a tourist. “I and Dad put it untouched and put a bed in the back,” Ashley says.
There are pictures of Emily and Ashley on the walls, which are in the form of young children next to the huge carved Halloween pumpkin.
Dr. Moore is still hitting Wayne’s hand and sometimes checking her pulse. For a person who says Emily, “always walking, always, always active, always active”, these are the last moments of the journey of life who is surrounded by those who matters the most to them.
Dr. 12.22 pm Moore says, “I think he has passed … he is now in peace.”
Outside, the mockingbird is silent. “No more pain,” Stella says, hugging her children in her arms.
I step out to give the family some space, and have reflected and filmed what we have just seen.
I have been covering medical morality for BBC for more than 20 years. In 2006, I was present outside an apartment in Zurich, where a retired doctor Dr. Anne Turner died with the help of group Dignitas – but California was the first time I was an eyewitness to an auxiliary death.
This is not just a story about the death of a man in California – it is about this that in England and Wales can become a reality here for those who qualify for a supportive death and choose to die in this way.
Whether you are for the proposed new Westminster law or the death of a loved one is a deep personal and emotional time for a family. Each death leaves an imprint, as the will of the vein.
Additional Reporting by Josh Falcon



